Case details
55 day old baby admitted with excessive cry and low grade fever for 2 days. First born baby to 29 year old father and 22 year old mother conceived within four months of marriage. Antenatal period uneventful. No history of fever, rash, drug intake. No pregnancy related or other medical disorders in second and last trimesters. She had usual antenatal care with injection tetanus toxoid, iron and folic acid tablets. Weight gain normal. Antenatal ultra-sonogram was normal. Delivery normal at full term with 2.8 kg birthweight. She cried immediately after birth, started feeds normally. During routine check up doctor detected heart murmur and was investigated by a cardiologist and later referred to Sree Chithra Thirunal Institute. After work up, the baby was on put on drugs in syrup form to be taken daily. Mother did not notice any problem in the first four weeks. Feeding was normal, no bluish discoloration. Gaining weight in the first 4 weeks was adequate. Since last three weeks mother noticed feeding difficulty in the form of suck rest cycle and slowing of weight gain. She also noticed head sweating. His development is proceeding normally .
No family history of any congenital heart disease .
Immunization is upto date
Now baby is admitted for low grade fever and excessive crying. After getting admitted, provisional diagnosis of acute otitis media was made and is now put on oral antibiotics. Fever subsided next day and no irritability now .
Before we proceed further, few points for Undergraduates:
Obviously why this baby landed up here now is unrelated to the problem which the parents are worried.
" Sir, is it related to his heart condition ?
Can you say - " NO " without a second thought ?
Before you reassure the parents, consider few entities related to heart which can be one of the manifestation of heart problem. Here, baby is brought with inconsolable cry. Parents complained of excessive head sweating already. In that setting especially when the baby was all right up to four weeks, one entity to be kept in mind is an 'ALCAPA' ie Anomalous Left Coronary Artery Arising from the Aorta. This is the usual time of presentation of this entity. It usually presents with features of congestive failure. Baby with features of myocardial ischaemia and excessive cry can be one of the manifestations. Most of these cases there wont be any abnormal clinical findings in the newborn examination.
( Please read about this entity. Why late presentation, embryological basis of this entity etc)
Any way common things always common .
A patient coming with fever at this age, some infections or inflammations are more important entities eg: Acute otitis media, meningitis .
In our case it turned out to be acute otitis media.
One more condition when a baby with fever, irritability. excessive cry where we should consider cardiac cause for excessive cry is Kawasaki disease. Of course not common at this age, Kawasaki disease may present in an atypical form occasionally. Always check for other signs like redness of lips and eyes and if other diagnostic possibilities are excluded better to include ECG as an investigation? Irritability is part of the illness. Excessive cry and irritability may be due to cardiac ischemia
A patient diagnosed as heart problem in neonatal period coming with unexplained cry is to be observed for the possibility of cyanotic spell if there is any finding supporting for that. One point to be kept in mind is cyanotic spell does not depend on the severity of cyanosis in an individual case. Spell may be more prominent in a case with mild cyanosis and the other way cyanotic spell need not occur at all in a case with severe cyanosis.
Babies already worked by the experts is brought to you with some complaint, it is natural only for you to check the the papers and then proceed with your evaluations .Better try to analyse on your own without going through the papers. If you are in a busy OP or if patients general condition is unstable this is not practicable.
Now come to our case . Here what are the diagnostically useful points?
Stable new born baby was detected to have some abnormal clinical findings in the CVS exam, worked by experts and he was put on some oral medications and baby is surviving at 54 days
The possibilities are:
The possibilities are:
1. Congenital heart disease which does not need any emergency intervention, but need medications. May be their plan is to put the patient on medications and decide based on the response.
Just because he is on medications, we cannot say that it must be a structural lesion.
Most common scenario which we are familiar with are structural heart disease going in for failure, most common being left to right shunts and increased flow cyanotic heart diseases where we put the patient on decongestants vasodilators, digoxin etc
But other situations like arrhythmias and cyanotic heart diseases with decreased flow also may be put on long term medications like beta blockers and iron.
So don't be biased, it need not be diuretics and digoxin always.
Most common scenario which we are familiar with are structural heart disease going in for failure, most common being left to right shunts and increased flow cyanotic heart diseases where we put the patient on decongestants vasodilators, digoxin etc
But other situations like arrhythmias and cyanotic heart diseases with decreased flow also may be put on long term medications like beta blockers and iron.
So don't be biased, it need not be diuretics and digoxin always.
2. As no interventions done, we can rule out few of the possibilities like critical stenotic situations on left or right side, TGA without communication, obstructed TAPVC and other situation where baby wont survive without immediate intervention of some sort.
3. Baby did not have much of problems during the first four weeks and was gaining weight. So what drug he was put on in the first week ?
a. May be drugs for congestive failure which was adequate initially but dose not modified as he gained weight.
b.May be it is an entity where congestive failure starts later eg.VSD, Endocardial cushion defect etc where the onset of failure may be after initial normal period .
4.May be the diagnosed entity did not have anything to do with the dyspnea or failure to gain weight. Dyspnea and failure to gain weight may be respiratory or metabolic and just because he was worked up in a higher institution for cardiac condition we attribute everything to cardiac condition. May be it may be a benign murmur or few of other benign situations as in small ASD, valve prolapse, bicuspid aortic valve etc.
Asymptomatic period of initial four weeks helps to rule out few other reasons of dyspnea also . Most of the respiratory causes of dyspnea baby can not be totally asymptomatic during this period .Commonest reason for this late onset dyspnoea is pneumonia , in this case unlikely . ( persisting from 30 days to 54 days with mild dyspnoea and no fever. Ocasionally lung malformations like congenital lobar emphysema , Cystic adenomatoid malformation , sequestration lung etc may present in this manner .
What about a metabolic cause responsible for dyspnea? Inborn errors of metabolism with metabolic acidosis usually they start to manifest earlier than . Alos there are not much points to suggest this possibility here.
So what remains as cause for dyspnea here ?
So what remains as cause for dyspnea here ?
Suck rest cycle starting from one month of age must be due to congestive failure situation itself. underlying condition of heart is one which becomes symptomatic gradually after first few weeks .
What are the entities to be considered which ll fit with the above situation?
1. Common things always common , left to right shunt VSD , moderate or large is the classical example . They usually presents after a gap . ( please read why they present after a gap even when the size is large.One important point to remind you is just because a baby presented with failure in the early newborn period we cant say it is unlikely to be VSD . VSD can present at that age also in special situations
2.Most of the cyanotic heart diseases with increased flow presenting with failure do so earlier then this .
Other rarer causes of congestive failure like Pompes , carnithin and other causes of Dilated cardiomyopathy , severe anemia , thyroid dysfuntion , hypertension arrhythmia's are to be considered and ruled out by clinical clues .
Now come to the examination findings
Other rarer causes of congestive failure like Pompes , carnithin and other causes of Dilated cardiomyopathy , severe anemia , thyroid dysfuntion , hypertension arrhythmia's are to be considered and ruled out by clinical clues .
Now come to the examination findings
Baby active playful. There is tinge of bluish discoloration of lips which increased on crying. Weight was 3.5 kg ie,700 grams over 50 days. About 15 gram per day on an average . According to history this sluggishness in the weight gain is over last four weeks .
Pulse rate was 120 per minute Respiratory rate 40 per minute , no in drawing of chest or noisy
breathing.
Respiratory system exam. RR 40 per minute , no in drawing of chest wall Chest movement normal ,apex of heart not visible. Air entry equal on both side ,no abnormal or added sounds
Cardiovascular system examination findings
Pulse normal volume ,all peripheral pulses palpable BP not checked
JVP , not seen
Pre cordial exam .. No pulsations over precordium /jugular or epigastrium . Apex palpated fifth space in the mid clavicular line on the left side not forceful . That means there is left ventricle dilatation .No thrill ,no pulsations felt in suprasternal and epi gastrium
On auscultation First heart sound normal ( pan systolic murmur is there starting from first sound still it is clearly made out ,second heart sound normal intensity single in the pulmonary area .Third heart sound in the Lower left sternal border and apex .There is a pan systolic murmur grade III maximum internsity in the lower left sternal border .There is a mid diastolic murmur in the lower left sternal border and apex ( almost equal intensity in the two areas
SO
Step wise analysis .
1.There is tinge of cyanosis , no doubt .
2. Cyanosis is not due to peripheral causes , it is central cyanosis
3. Respiratory causes of cyanosis ruled out as there is no dyspnea at rest to account for it and findings does nt support
4. Cardiac causes Left right shunt with reversal ? Less likely at this age
So we are dealing with a case of cyanotic heart disease .
Basically there are two types, decreased flow and increased flow state.
Important ones in the decreased flow state are Fallots, DORV with PS , Single ventricle with PS , Ebsteins anomaly TGA ,VSD with PS.
Important ones among increased flow states are TGV with or without VSD ,DORV without PS and Single ventricle without PS , TAPVC ,Persistent Truncus .
How to differentiate between them and which of the above category our case belong to ?
Any features of failure and mild cyanosis argue for the increased flow state . In this group TGV even with VSD will have noticable cyanosis . All the others cyanosis ll be mild and we may miss cyanosis
Any spell , severe cyanosis and absence of features of failure argue for the decreased flow states . In this group ebsteins anomaly cyanosis may be mild .
Our case there is no history of spell so far .Baby is not dyspnoic but from mothers history there is suck rest cycle and failure to gain weight both of them should be taken as evidence of failure. So it is an increased flow state CCHD
So from the above list of entities which is fitting here ?
Out of the increased flow group TGV without communcations is ruled out for sure . they wont survive beyond hours without any intervention. No intervention so far
TGV with VSD ? Yes possible . But more points against this possibility . They ll be more symptomatic with features of failure dominant and the cyanosis with whatever mixing happening through the vsd , will be much more than this
Out of the other situations with increased flow state , TAPVC without obstruction is the more likely situation .
DORV without PS , Single ventricle without PS , Persistent truncus are possible but rarer situations . One point difficult to explain in all the above situations is the comparatively asymptomatic state in the first month .
One entity possible here is Endocardial cushion defect which ll present some where in the third or fourth week .
So what does the clinical findings suggest
Pulse and BP reflects the left side of heart and JVP reflects the right side . In the evaluation of cyanotic heart diseases JVP analysis is more useful than analysis of pulse and BP.
Few clinical useful points of pulse examination in a case of CCHD
High volume collapsing nature of pulse in persistant trunkus
High rate and irregularity in ebstein as a rare complication of SVT in associated Pre excitation pathway
Absence of radial pulse in case where BT shunt is done ,or due to embolic phenomenon .
Out of this in our case only useful point is pulse volume . We are considering persistant trunkus as one possibility . In this case pulse volume is normal .
Pulse and BP reflects the left side of heart and JVP reflects the right side . In the evaluation of cyanotic heart diseases JVP analysis is more useful than analysis of pulse and BP.
Few clinical useful points of pulse examination in a case of CCHD
High volume collapsing nature of pulse in persistant trunkus
High rate and irregularity in ebstein as a rare complication of SVT in associated Pre excitation pathway
Absence of radial pulse in case where BT shunt is done ,or due to embolic phenomenon .
Out of this in our case only useful point is pulse volume . We are considering persistant trunkus as one possibility . In this case pulse volume is normal .
Precordial examination showed LV enlargement , No RV impulse , percussion not done to elicit RA enlargement or pulmonary area .
Among heart sounds analysis of second sound is the most important in case of cyanotic heart disease. Out of the possibilities considered TAPVC , Endocardial cushin defect was high in the list , but one strong point against these two possibilities Second sound is not wide split , In our case it was single or narrow split .
One useful asuculatory finding is diastolic murmer in the lower left sternal border and apex. What all conditions in this situation we ll get diastolic events .
1. Regurgitation from Persistant trunkus or Pulmoary regurgitation in rare variants of fallots ( absent pulmonary valve . Remember in Persistant trunkus there is one common valve which ll be in competent in 90 percent of cases . So a single closing sound and a regurgitant murmur with high volume collapsing pulse are the rules in a case this high flow cyanotic heart disease state . Both these situations diastolic murmer will be early diastolic one with a high pitch
2 in this case the murmer is low pitch middiastolic murmer , If we get it in the lower left sternal border in a case with tinge of cyanosis possibilities are 1. TAPVC where the high flow across the tricuspid valve causes MDM as we get in ASD .
B Any situation with Tricuspid regurgitation , PAPVC also we ll get this , In TR we ll get Pan systolic murmer and MDM
C Ebateins anomaly multiple sounds in diastole at this area may mimic this entity , Also the systolic muremur of Tricuspid regurgitation can occur
So out of these what is the likely reason in this case ? What is common for the first two situations is the prominent right ventricle . In TAPVC there is volume overloaded right ventricle , in TR most of the cases are due to high outlet pressure the RV ishypertrophic . In our case we did nt get RV impulse
Is it ebstein ? Can Ebstein be considered in a case where we consider high flow cyanotic heart disease ? Yes . In few cases pulmonary vascularity may be high .
Few very valuable points which we could nt make sure are JVP , RA enlargement we tried to elicit but could nt make out .In ebstein usually we get a comparatively silent precordium . Even though the diastolic clicking sound is described we rarely get this prominent murnur .
Above all one question remains. What is the reason for the MDM which is prominent at the Apex ?
So at this stage , where are we
At the end of clinical examination we had TAPVC and ECD as first possibilities , After clinial examination few strong points arguing against both possibilities. In ECD we get all chambers enlarged. Second sound ll be split . In TAPVC , Right atria and right ventricle ll be enlarged. Here right ventricle not enlarged and LV is enalarged. Second sound is not split . There is one point favoring TAPVC ie MDM at the Lower left sternal border.So most of the points argue out these possibiities
We considered persistant trukus , but here no high volume pulse , no regurgitant murmer. It is out
Can it be single ventricle or DORV there is systolic murmer which is common in both . But very difficult to explain the mid diastolic murmer which is prominent finding.
Many of the findings are favoring Ebsteins anomaly , but history wise our case is one of high pulmonary flow state
So
At the end of our clinical analysis we are nowhere
Investigations
Not a good film .But cardiomegaly with LV enlargement and increased vascularity . So it is one of the increased flow states.
Thymus not prominent .
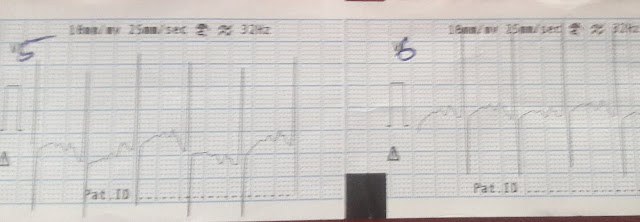
ECG

Rate 120 , rhythm regular . Prominent P waves duration almost 3 divisions ,duration almost 3 divisions ie right atrial enlargement , left atria also .PR interval normal , QRS morphology does nt show any evidence of pre excitation.

Axis left .
Prominent LV , No RV forces
So out of the possibilites we considered all the entities with RV enlargement and RV forces is out. ie TAPVC
Entities with this negative axis
1. Ebsteins anomaly
2.Tricuspid atresia
3.Endocardial cusion defect
Out of this entities Endocardial cushion defect many points are against in clinical examination In the ECG we expect RV forces
Out of the first two both can cause Left axis. Prominent Right atria Promiennt LV forces and atretic RV. so ECG is consistant with Either of the two .
But clinically Out of the two both are decreased flow states . If at all ebsteins can occasionally lead to Increased flow and cause congestive failure.
So at the end
We considered possbility of Ebsteins
Now what was the ECHO finding?

First ECHO from periphery . this is the reference letter to Chithra
with the ECHO result which of our finding can be explained.
1. Onset after a gap can be explained
2. Failure with a tinge of cyanosis can be explained
3. Cardiomegaly , but we expect RV forces which is not here
4. Split second sound , not here , which is almost always the case. Is it because of early PH. ? No . RV forces are not there
5. Left axis argues of osteum primum ASD or ECD . it need not always be right upper quadrant axis
This case was worked up in Sreechithithra

So where are we now
We never heard of a Tricuspid atresia case causing flooding of lung , causing pulmonary hypertension
One doubt here , when the RV is atretic and pulmonary hypertension develops
So not at all conviced with the arguements
Our arguements were
When the Tricuspid valve is atretic the source of blood to pulmonary circulation is through VSD or PDA . from the blood which reaches the left ventricle from two sources. Can this flood the lung when it takes a devious route through VSD or PDA ?
We did an ECHO from our institution also
Findings were agreing to the above
So we learned from mistake
ie .
In tricuspid atresia also rarely there is a possibility of pulmonary flooding if the communication is large and it can behave like an increased flow state.
Anatomy described in the above ECHO ie almost single atrium , allows the blood flow freely to LA . , then to Dilated LV . Here the VSD is so large that it behaves like a single mixing chamber. In that context a low resitance pulmonary vascular system blood takes the less resistant pathway .
One question remains un answered
What is the reason for MDM which we heard very well and that was the main point discussed and we approached the case based on this finding .
For MDM in the Lower left sternal border there should be either smaller than normal patency of the tricuspid or higher than normal flow across the tricuspid valve. Here in Tricuspid atresia whole aperture here is closed . So both of above can serve as an explanation.. In Tricuspid atresia here ASD is so large that it looks like single atrium. So the volume of LA is twice the normal , So the flow across the Mitral is much higher. May be this higher flow across the mitral caused a flow murmer MDM at the apex and the same murmur heard in the lower left sternal border.
Fine , that is a good explanation .
But if some body ask back.............Sir , what is the situation in Ebsteins and Tricuspid atresia . the same is the case in all case of tricuspid atresia and ebstein always. In your case if it is taken as an explanation this finding should be there in all cases of TA and Ebstein. But it is not there .
What may be the reason ?
My postulate .........In TA and Ebstein in most of the cases LA is so large and Mitral valve annular dilatation just like what is happeing in Dilated cardiiomyopathy and mitral valve is no more small , so not much of MDM . If the LV is not large due to any reason as in this case annular dialatation may not be significant and this can lead to MDM
This is just a postulate.
We ll wait for experts comments and criticism for our findings , our explanations and wild postulations