Case presentation Patient reported on 24 /10 at 7pm .Seen by me on 26 at 8 am
8 year old girl child previously normal had low grade fever three days back , controlled with paracetamol. Yesterday developed generalized tonic clonic seizures . .Had mild head ache , vomited once before this. Parents were not sure about the onset progression. As the seizures not controlled with anti convulsants she was referred to us yesterday night . Managed as status epilepticus in PICU ( dilantin loading , and valproate infusion )
She was born at term ,no significant perinatal events , development normal going to school average in scholastic performance.
No fever, weight loss .
No contact with Chronic cough case. no travel outside .
No family history of seizure mental retardation
No history of trauma, no significant bleeding diathesis
Chance of drug consumption unlikely
Immunized update .
I saw her today morning .
She was conscious ,behavior abnormal ,crying and laughing .In between seems normal , Mood swings frequent .
BP 96-60 . Pulse 80 /mt ,normal in rhythm,volume Temp 98 F ,Breathing normal in depth 20 /mt
She is ill nourished ( both weight and height , not recorded
No significant pallor .
No Injury on scalp,No ear discharge.
No significant lymph nodes No rash or bleeds on skin .
No neurocutaneous markers
No abnormal movement ,Moving all limbs .
(She took one dosha and tea , but vomited. She slapped the staff nurse when she tried to give IV inj)
CNS
Heigher functions , emotional and behvioural alteration as mentioned. He told her name ,but no more answers to other questions.
Craneal nerves , which could be tested. Eye no ptosis , no nystagmus , movements normal. Pupils normal size and reaction Fundus normal , no bleeds
Other craneal nerves normal
Motor system,tone ,power reflexes normal , Yesterday her planter was upgoing , today down going both sides.
No signs of meningeal irriation
Skull , spine normal No bruit ,Crack pot sign neg
Cerebellar signs obviously not there ( she had dilantin bolus .)
Other systems
P/A. Liver , spleen not palpable No other mass , no distention NO free fluid
Chest clear
CVS normal
Thoughts at this stage? teaching points
Previously normal child developing fever followed by Generalised tonic clonic seizures ,where most of the other reasons negative
1. Infection .
2. Metabolic error triggered by infection
3 Central demyelination/immune encephalitis
4.Connective tissue disorders/malignancies
Out of this chance of infection is highest .
Among the infection, bacterial and viral highest . Tuberculous ,malaria or rarer organisms like ricketsiels
Here fever is not high grade, patient not toxic .No signs of meningeal irritation
In the absence of pallor , No spleen malaria less likely .
So out of the infections viral infection was top in the list , then bacterial infections .If the patient had antibiotics from outside partially treated pyogenic meningitis would have been a closer DD. Here patient was not put on any antibiotics. No features of immunocompromised state. So by the time this much of features of parenchymal involvment (seizure ,behaviour problem without Raised ICT ) we expect signs of meningeal irritation in case of Bacterial meningitis. So order of possibilities among infection Viral first.
Out of the viral infections , Herpes and Jap B are the commonest in our areas and Herpes major treatable entity . Features which will help to differentiate between these two are 1. Focal seizures more likely in Herpes. 2. History of smell abnormalities if elicited suggest herpes. 3.Extrapyramical signs in Jap B .( but need not be early )
Investigations
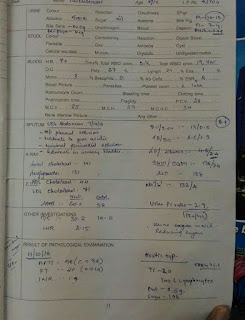
Blood . Total count 16000,DC neutrophil 74, Lymphocytes 24 ,Eosinophil 2.
ESR 10
Serum Calcium 9 , Sodium 135 , Potasium 4. Blood sugar 116 mg /dl
LP done. CSF pressure normal , Clear ,Cells total 60 , Neutrophil 20 per Lymphocytes 80 ,No RBC
Sugar 84, Protein 50 .
CSF collected and sent for virological studies and CBNAT
So where are we now ? after the basic investigation results
Metabolic , electrolyte abnormalities ruled out
CSF contains Cells . Lymphocyte predominant
So ?
Infection
ADEM
Questions here .
Out of the infections which will be first possibility ?
ADEM can it present this way .
Very important to decide clinically as Final confirmation with investigations will take time. We wont get MRI today . We wont get Viral studies result today . Putting the kid covering all these possibilities is possible but does nt seems good , Can you rule out or narrow down further and decide what should be the drug of choice.
If you are asked to choose just one drug out of Antibiotics, Methyl pred. Acyclovir or Antituberculous
Pyogenic meningitis ?and putting on Antibiotic . Points arguing for jpyogenic meningitis
Total count High. Neutrophil predemonance ? Good , but what about ESR ..it is 10 .So which way to go , Leucocytosis with neutrophilia argues for PM. but this low ESR very unusual , which of this is to be given weight ? I ll give more weight for normal or Low ESR . The negative predictive value of this is more useful point against PM than the leucocytosis with neutrophila. ( Viral infections occasionally cause this blood picture But high ESR less likely in viral infection ,So viral infection is a better explanation for this Count and ESR
CSF picture
Cells are there. count less than 100 ,predominantly lymphocytes , but some neutrophils. This LP done on the third day of illness.
, Yes you may get this picture in pyogenic meningitis , but usually if patient is exposed to antibiotics. Usually the count is higher than this by the time patient presents with this clinical state. One more point , CSF sugar is normal and the ratio with blood sugar is above 75 percent .Above all patient is not having high grade fever , toxicity . Even though it is treatable entity pyogenic meningitis possibility in this case is less likely
Will you avoid antibiotics altogether in this case ?
No , because in medicine unless we are sure about diagnosis , You cant take a decision not to give treatment for a treatable common entity . So i ll put the patient on Antibiotics at this stage. May be i ll stop when i get a stronger evidence against this or more points for other possibilities
Is it virl meningitis or Viral encephalitis ?
Viral meningitis Pathology is mainly meninges with or without minimal brain parenchyma involvment . So features usually are signs of meningeal irritation , raised ICT , but less of focal neurological deficit or seizures. ( Of course these are not hard and fast rules. )
Viral meningitis , usually no meningeal inflamation, more of parenchymal involvment So less chance of meningeal signs, more chance of focal deficit seizures and altered sensorium in the abscence of raised ICT .
In our case more chance of viral encephalitis. than viral meningitis
What is the chance of TB meningitis . Yes CSF cytology argues for it . There can be initial neutrophils even though after 72 hours it ll be replaced fully by lymphocytes. Count of cells used to be little higher , but wont be that high as pyogenic. But biochemistry is not supporting. No rise in proteins
Clinical presention of TBM is usually bit slow ( it can present acutely also ,but rare ), No contact with TB , no lymph node, no Chest signs. Not many points supporting this .
Malaria ? NO , no pallor , no spleen
What is the chance of demyelination and other immune encephalopathies.?
Possible , and to be considered in this case . Points in favor are low grade fever , which disappeared now. . It can present with seizures. behavioural abnormalities. CSF picture supports.
So at this stage Till we get an Imaging ADEM is high in the list
Other immune encephalopathies like NMDA receptar encephalitis , a bit unusual , the seizures charecteristic peri oral movements not present here. Still one of the DDs at this stage
So what drug put on at this stage
At this stage patient was put on Ceftriaxone only ,
Ideally at this stage Ceftriaxone and Acyclovir are to be started imperically , But as the seizures were under control , and the general condition stable , I decided to get an MRI at the earliest .
MRI .We got after 12 hours of this
So main DDs were between Encephalitis and ADEM .
Findings ..There is a hyperintense lesion on the right tempero parietal ares , with local dilatation of lteral ventricles. It is not related to this event. Probably an old lesion
There is diffuse hyper intensity frontal base and temporal area on left side .I am not able to comment on the diffusion and perfusion restriction images.
These lesions are more suggestive of encephalitis , most probably herpes because of location and the diffuse nature. Less points for ADEM . Basal ganglion not affected argues against possibility of Jap B
So ..
Now patient is put on Acyclovir and Ceftriaxone stopped.
There may be difference of opinion , is it fair to cut Ceftriaxone . All of us agree with starting of Acyclovir. Most of us may not consider putting on methyl pred.
But stopping ceftriaxone? ..
My decision is based on taking whole picture. Considering many points starting from clinical picture , CSF , MRI. chances of Pyogenic meningitis are very unlikely .
So let us see ..
26/10/2016
8 AM
She had generalised seizure at night ,controlled with lorazepam. Now febrile. neck stiffness +
One finding which we missed yesterday became more prominent today
Small grouped vesicles ,of herpes .
As the kid looked sick , even though diagnosis is 99 percent herpes encephalitis , we restarted ceftriaxone. ( yesterday she got morning dose ceftriaxone, and skipped night dose )
We could do EEG today
3/11/2016
12th day
Fully conscious , afebrile .no focal deficit
Follow up