Bought now with pale stools since newborn period, edema and abdominal distention for the last month .
No antenatal problems in the form of exposure to terratogens or infections,no meternal illness,delivered at term normally with a birth weight of 2.7 kg .Baby not asphyxiated breast fed normally . Mother complained of jaundice from third day ,urine was normal .She says the baby had pale stools at that time. No blood group incompactibility .Baby was active was under phototherappy for three days .From the fifth day onwards vomiting started which was nonbilious . Bowel was normal , no abdominal distention . No history of seizures no altered sensorium. Did nt notice any unusual smell or color of urine or body .He did nt gain weight in spite of feeding normally . ( Mother successfully breast fed the first baby and her feeding technique was normal ) . As this combination was suggestive of inborn error of metabolism he was investigated but no conclusion . As the jaundice subsided by end of first week, vomiting by the end of second week. Baby was discharged on breast feeds.
Next visit was at three months with pale stools and discoloration of urine noted two days prior .Baby weight was 4.3 kg .Since then stool remained pale ,urine yellow baby did nt gain weight and for the last one month further loss of weight ,abdominal distention and odema both legs .
No alteration of sensorium ,no seizures any time.
No bleeding manifestations.
Teaching point for PGs
Very important point here is to answer the question when is the onset of this problem .In the newborn period there was vomiting ,jaundice and now again the jaundice reappeared with definite pale stools abdominal distention and odema. One thing is clear there is a cholestatic liver disorder with decompensation of liver function which is fast progressing in an early infant .We are tempted to say the onset is from new born period
But few points argue against this idea. Jaundice disappeared on the seventh day and it was not there till three months. Vomiting disappeared by end of second week. Above all baby gained weight from 2.7 to 4.3 by the end of third month.Mother says stool color was white. Here you have to take a decision , which of these points to be relied on . If a cholestatic disorder had an onset on third day and the yellowish discoloration of urine did nt persist the stool color she says must be wrong. This is one point to be remembered. a mother is likely to attribute the present problem had a relation to the newborn period .In this case most likely the problems in the newborn period both the vomiting and the jaundice are unrelated to this problem which has an onset and gradual progression from three months. That may be sepsis , or physiological jaundice with another problem responsible for vomiting .
O/E
Breathing normal (not acidotic) ,circulation stable,Irritable .Pedal odema .tinge of jaundice in eyes ,marked wasting around groin axilla,abdomen spine Abdomen distended shiny .
Teaching points
Assessment points in GE
Vital signs .Not only for stabilisation ,but may give diagnostic clues
Findings which gives diagnostic clues
Complications and sequel of the problem ,to assess the extent .
Vitals...Altered sensorium in this context ,argue for hepatic encephalopathy, IC bleed, electrolyte imbalance
Breathing Acidotic argues for the type of metabolic abnormalities which may be responsible for the hepatic involvement .
Cirulatory status . If baby sick argues for sepsis
Clues towards diagnosis in Cholestatic liver disorder .In this case no dysmorphic features. ( If there is abnormal look malformation type possibility of trisomies, watson alagille ,zelweger synrome and few other intrahepatic cholestasis )
In the eyes , apart from abnormal dismorphic features cataract ,relevent for galactosemia ,Intrauterine infections , trisomies .
Look for other features of intra uterine infections.
Head size may be abnormal in IU infections and genetic disorders
Hypothyroidism .
Findings which helps to assess the extent of problem and compli
Features of nutrient/micro nutrient deficiency due to malabsorption, eg wasting,bleed , rickets.vitamin E ,Vitamin A deficiency . So look at the eyes for bleed, vitamin A def . apart from the findings which already discussed
Skin for bleeds , rash ,lipid deposits ,scratch mark in an older child, findings in relation with nutritional deficiency . Few of metabolic disorders also may leave some clue on the skin .
Head.. Wide AF and features of rickets. Palpate fontanels not only for rickets but for bulging due to Intra cranial bleed. Rickets a bit unusual if associated malnutrition is severe
Tone of baby is important . Hypotonia may occur in many of genetic syndromes with cholestasis,nutrient deficiency .
In this baby skin was normal . No bleeds , rash
Now very important findings which are relevent for diagnosis in this case. The limbs were spastic and bit rotated position , suspicios of dystonia , cortical fisting.
Development assessment also interesting. Here there is significant motor delay. ( head control not achieved , not only that other field also delayed. If it is a isolated liver disorder development delay usually in gross motor field.
When we get delay in other fields it suggest it affect Nervous system also , many entities which cause this considered here eg hypothyroidism , intra uterine infection , Inborn error of metabolism which affects brain and liver cells simultaneously .
Here one point to be discussed is .. kwoshorkor , in a baby who is not gaining weight , odema, one of the treatable entities is malnutrition either protein calory or other micro nutrients like zinc, iron ,thiamin all of which may cause odema
Here this baby is not apathetic , but irritable, No skin lesions both of which are imp to consider kwashorkor . One very imp point is abdominal distention. ( System exam showed free fluid ) very uncommon in Kwashorkor unless other complications like Tuberculosis . So malnutrition may be contributing, but not per se responsible for this odema
About possibility of anemia as cause. No , baby not that pale and he is not dyspneic. By the time anemia causes odema patient ll have all features of congestive failure
Gastro intestinal system
Abdomen grossly distended , shiny abdomen dilated veins mainly sides of abdomen and chest , flow of veins can not be made out easily. All tests of free fluid positive, Liver , spleen not palpable , scrotal odema
So where are we now. ( We are yet to examine CNS which i ll consider after bit of discussion of the features we got so far . I ll try to link the CNS findings at the end )
A case of liver problem may present
1. No symptoms , just palpable liver , with or without spleen.
2. Features of liver dysfunction eg jaundice, bleeds. odema , encephalopathy
In the first category Just consider the structure of liver and how it can be enlarged. eg ,hyperplasia of cells, reticulo end system, congestion of vein , or bile tree. infliteration of inflamatory cells, infilteration with fat or glycogen ( all of the above cause soft enlargement , Infilteration with malignancies or storage meterials other than glycogen lead to firm liver . None of the above interfere with hepatic cells. They just invade without interfering with cellular organells , So just hepatomegaly . If somehow above pathology block the portal system spleen also enlarges. Spleen may be enlarged in some pathologies which affect liver and spleen both eg viral infectionsn leukemia , malaria etc
Second category . Features of liver cell function derangement . What that mean , liver cells are damaged. This again depends on to what extent it is due to bilary tract pathology , to what extent cell damage. Pure duct pathology jaundice and fat soluble vitamin deficiency , but no features of cell damage. Cell damage later.
If cell damage early we ll get featurs of failure.
The above pattern reflects the biochemistry also . Cell injury leads to release of transaminase . No injury , but canal block more of other enzymes like alkaline po4 ,GGT etc
Here features of decompensation , and liver not palpable. means liver cells are damaged .
So the type of liver problem is progressively damaging the cells .
We need not consider entities which lead to storage only .
What are the examples of these groups.
Classical is galactosemia,
Next tyrosinemia
Fructose intolerence
Hemochromatosis
Commonest one is galactosemia. In this case is it galactosemia
No . the onset is early , progress fast. Here no hypoglycemia, no cateract.
Tyrosinemia , hemochromatosis ..possible
alfa one antitrypsin deficiency .. Possible but usually a bit late onset and slower progress
PFIC .. possible but slow progression and more of cholestasis
Now We ll try to assess the CNS
Development assessment shows delay in other fields also. In the limbs there are features of spasticity and dystonia .
So at the end
Metabolic liver disorder with early onset and fast progression to decompensation , with CNS involvement , diffuse . interstingly extrapyramidal also
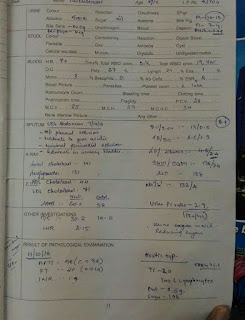
Investigations
Now after investigation ?




Great discussion...sir I hav narrowed it down to a metabolic liver disease which affect the Cns as well..as u said galactosemia is out.other possibilities are tyrosinemia .neonatal hemochromatosis.but that presents with very hard liver if I remember correctly.rare condition citrin deficiency?...it is very intriguing..please discuss further..very interesting case..ur analysis is super..
ReplyDeletePlease read you have narrowed it down to...
ReplyDeleteThank you Rajkumar .Galactosemia progresses very fast. Thyrosinemia variants are there which may present late also . Neonatal hemochromatosis we had. this entity is very important because IV GAMMA may give releif.
Deletei dont know about Citrin deficiency . Have to read.
Patient is in ICU. shall let you know follow up
Thank you Rajkumar .Galactosemia progresses very fast. Thyrosinemia variants are there which may present late also . Neonatal hemochromatosis we had. this entity is very important because IV GAMMA may give releif.
Deletei dont know about Citrin deficiency . Have to read.
Patient is in ICU. shall let you know follow up