11 year old girl who was healthy till one week back had low grade fever followed by focal seizures on right side. Seizure lasted five minutes.She regained consciousness but recurred after few hours. Fever subsided with one dose of paracetamol and lasted one day only .
No past history of significant illness,
No contact wit PT, no ear discharge, head trauma
Born our of non consanguinous marriage,Antenatal ,natal postnatal period uneventful
Development all normal ,
Immunised update
No family history of any neurological disorders
On admission altered sensorium ,
breathing normal ,
BP 110/70 ,pulse 80/min,afebrile.
No bleeds ,rash jaundice .
Eye movements normal ,pupils normal size and reaction fundus normal .
other Cranial nerves normal
Motor system ,power normal ,tone lower all limbs reflexes sluggish ,plantar up going
No signs of meningeal irritation
Provisional diagnosis of ADEM /Herpes encephalitis was made
First level investigations done
LP done , CSF clear ,normal pressure
With this Possibility of Encephaltis was high in the list and considering treatable encephalitis patient was put on Acyclovir and supportive measures
Teaching points
Patient had mild fever at onset only and dominant fever of encephalitis possibility of bacterial /tuberculosu meningitis not considered high in the list.
With the blood and CSF result also was not favoring. we did nt put the patient on antibiotics.
( This is a major decision , in an ICU setting with altered sensorium focal seizures and CSF showing cells it is dictum to put patient on treatable drugs , life is more important and time too short. So usually we take a policy to start management of pyogenic meningitis , acyclovir . At the same time send for virological studies , cultures. A policy to start this and stop later once the possibility is disproved. That ll be a better decision in an ICU . Here many points arguing against pyogenic or tuberculous and we took a decision not to start imperical antibiotics or ATT , but acyclovir only .
With evidence of diffuse brain involvement ,no fever possibility of biochemical /metabolic , toxic /system function derangement to be ruled out .
Here biochemical report did not support any of them . ie blood sugar ,electrolytes ,RFT ,LFT .Possibility of poisoning ,no circumstancial or clinical supporting evidences .
With the CSF finding of Lymphocytes possibility again increased for possibility of infection . But this may be misleading , the cell number is low , only lymphocytes. This can happen following any seizure.
Argument for Herpes encephalitis usually are , cells , lymphocytes but more important is RBC in atraumatic LP . Here RBC were not there. Protein minimal elevation and sugar normal
We sent the CSF for Virological studies .
Next day patient developed this movements
(consent taken from parents in writing )
These were abnormal movements ,(not seizures ) repetitive involving left hands picking hair and dress. Abnormal movement around mouth was prominent. Encephalitis with extrapyramidal movements were suggestive of Jap B encephaltis . But this movement is more suggestive of another entity - NMDA receptar encephaltis . In fact many cases earlier were diagnosed as Jap B encephalitis before this entity was not known .
With this possibility in mind we send the CSF for NMDA receptar antibody and
She was Put on Methylprednisolone and IVIG ( better to give both in this condition )
MRI was taken next day
This was the report from radiologist , but i think there is some basal ganglion hyper intensity in flair images
NMDA receptar antibody result came as high titre positive
CSF virological study results from ICMR lab Manipal reported herpes , Jap B Dengue , westnile viruses negative .
Sensorium improved , but she had seizure on the third day . She was put on Levetirazetam
Since the last two days the abnormal movement worsened and sensorium deteriorating. Possibility of levetirazetam worsening the situation it was stopped and she was put on dilantin sodium . Short period she was on midazolam drip
Movements are less today , but the sensorium same.
Today She is put on Rituximab. 375 mg per meter square . 500 mg per day IV.
For the abnormal movement she is put on Tetrabenazine 25 mg half tab BD.
Supportive measures continuing. Nutrition fluid ,electrolyte balance maintained mainly be IG tube feeding .
In this context just sharing experience with few cases of NMDA encephalitis came to us during last two years.
First case of NMDA was not diagnosed as we did nt give importance to the movement of his face , he was managed as jap B encephalitis . Only after two weeks this possibility was known , We send for NMDA receptar antibody , we managed with IVIG , no response. Later he responded to IVIG plus methylprednislone. Later he was investigated for underlying conditions like gonadal tumors , All negative. He was put on Azathioprim , Now asymptomatic
Another boy diagnosed early because of this experience. but did nt respond to IVIG plus methylprednisolone, We could mobilise Rituximab in govt set up Weely once was given four doses.
He recovered , He also is under followup now on Azathioprim
Shall update
Please read
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2607118/





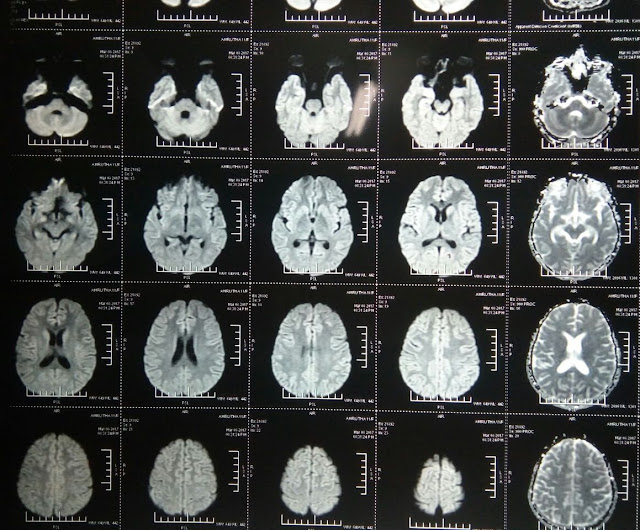







Sir, I didn't see BG signal, may be thalamus is bright.Some recent case report had reported seizure like activities with cefalosporins.
ReplyDeleteMyoclonus and encephalopathy can be drug induced as well. That should also be in the differential.
Thank you Sauparnika. I am not sure what anticonvulsant to be given now. She had seizure i cant stop dilantin. but i am afraid this may also worsen
ReplyDelete